The biological bandage is an emerging option for keratitis, recurrent corneal erosions and more.
Inflammation, the first sign of wound healing, is also the hallmark of all ocular surface diseases. Uncontrolled inflammation leads to chronic pain and discomfort/irritation, delayed healing, more tissue damage and vision-threatening complications such as corneal scarring and haze. Thus, effective control of inflammation is an important strategy to promote healing.
In the past, our armamentarium mostly consisted of topical anti-inflammatory drugs, bandage contact lenses and, in some instances, immunosuppressive agents. While largely successful, these treatments may not always resolve the patient’s condition.
In these instances, use of amniotic membrane represents an option for treatment and regenerating corneal and conjunctival tissue. Here, I will discuss the role of amniotic membrane, the innermost layer of the placenta, in treating ocular inflammation.
Amniotic Tissue and Wound Healing
Investigators have described transplantation of amniotic tissue, harvested and preserved following delivery of a newborn by C-section, as one of the major new developments in surgery of the ocular surface.1
The unique cryopreservation method of AmnioGraft and ProKera (Bio-Tissue, Doral, Fla.) allows for greater retention of the membrane’s structural, physiological and biochemical properties responsible for its dramatic healing and easier handling intraoperatively. A dehydrated preservation process, as is used with other types of amniotic membrane, devitalizes and denatures these properties, yielding a graft devoid of active factors and that is hard to handle. Cryopreserved amniotic membrane consists mainly of four components: epidermal growth factor; keratocyte growth factor; structural proteins, such as laminin and type VII collagen; and several neurotropic substances.1 The key mechanisms of amniotic membrane in wound healing are:1,2
- Inhibits matrix metalloproteinases (MMPs) thought to be directly related to a variety of basement membrane and epithelial dystrophies.
- Inhibits transcription growth factor (TGF)-ß signal transduction in corneal and conjunctival fibroblasts to prevent scarring.
images
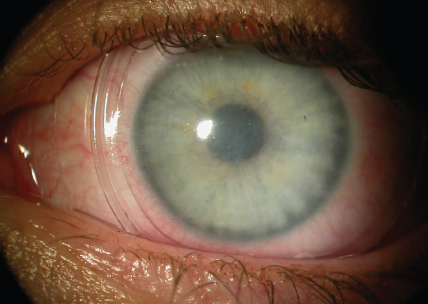
The ProKera bandage allows the ocular surface to retain its biomechanical healing properties.
- Reduces expression of various growth factors and pro-inflammatory cytokines, such as interleukin-1.
- Releases anti-inflammatory cytokines, such as interleukin-10.
- Promotes antiangiogenic activity.
- Retains some antimicrobial properties.
As a result, cryopreserved amniotic membrane relieves symptoms, promotes re-epithelialization and suppresses stromal inflammation, angiogenesis and scarring.1-3
Sutureless Amniotic Membrane
A sutureless form of amniotic membrane, ProKera, is a biological corneal bandage. This class II medical device is composed of cryopreserved amniotic membrane clipped into a thermoplastic ring set. It is FDA approved for corneal and limbal defects and scarring due to various etiologies. A 16-mm thermoplastic ring placed beneath the upper and lower lids holds the membrane in place and in direct contact with the affected area on the cornea.4
The amniotic corneal bandage has some advantages over an amniotic membrane allograft. The former can be inserted in the office rather than the operating room, and it requires no sutures. I’ve found that it allows for earlier treatment and, in many cases, quicker resolution of the signs and symptoms of corneal inflammation.5
Common indications for the biological corneal bandage include herpes simplex keratitis, microbial keratitis, filamentary keratitis, dry eye syndrome, recurrent corneal erosions and Salzmann’s nodular degeneration. Additional indications include corneal abrasions, scarring and erosions, chemical burns, corneal defects, partial limbal stem cell deficiencies, high-risk corneal transplants and Stevens–Johnson syndrome.
For Infectious Keratitis and Dry Eye
To achieve the greatest success with ProKera, one must first always treat the underlying disease process. When treating infectious keratitis with the amniotic membrane, I scrape the cornea to identify the specific pathogen, start fortified antibiotics, then use the graft as an adjunct treatment to enhance healing and reduce pain.
If the patient has exposure, you must perform a temporary tarsorrhaphy once the membrane is in place. This may be done by applying a Tegaderm (3M, St. Paul, Minn.) film dressing to the temporal aspect of the upper and lower eyelid, or, in more severe cases I like to use 6-0 prolene on a curved needle to temporarily suture the temporal aspect of the lids together, using a slip-knot technique for easier viewing of the patient’s eye during slit-lamp examination. For the patient with dry eye, ProKera is appropriate only after standard treatments, such as artificial tears, punctal plugs and Restasis (cyclosporine, Allergan, Irvine, Calif.) have failed.
Evaluating The Evidence
Various trials have shown that amniotic membrane—both as a graft or bandage — can successfully treat several of the aforementioned conditions. Among the most notable:
■ Ocular surface disease. Among 65 patients with different ocular surface diseases, one series reported that amniotic membrane transplants led to a reduction of pain, redness photophobia and inflammation with few complications.3
■ Varied corneal diseases and dystrophies. Researchers reviewed charts of 108 patients who underwent amniotic membrane transplantation (AMT) for nontraumatic corneal perforation, persistent epithelial defect, aphakic/pseudophakic bullous keratopathy, infectious ulcer resistant to treatment, necrotizing keratitis secondary to endophthalmitis or caustic injury.6 They found the mean survival of corneal integrity was similar in all groups, leading them to conclude that AMT is a successful adjunct in achieving corneal epitheliazation.
■ Conjunctival disorders. A trial evaluated 105 patients with corneal disorders and 25 patients with conjunctival disorders who underwent AMT and found that the cornea healed satisfactorily in 85.7% of the corneal group, and determined the success rate of conjunctival group to be 92%.7
■ Chemical and thermal injuries. Investigators analyzed AMT in 53 patients (53 eyes) with corneal ulceration and limbal deficiency following chemical and thermal injuries. They found the graft helped stop ulceration and promote corneal epithelialization in patients with severe chemical or thermal eye injuries.8
■ Stevens-Johnson syndrome and toxic epidermal necrolysis. Researchers at Loyola University in Maywood, Ill., found that early use of AMT prevents severe vision loss in these patients.9 A retrospective chart review of 128 patients admitted to the center’s Burn Intensive Care Unit found that one of 23 eyes with moderate or severe presentation treated with early amniotic membrane transplant had a poor outcome within three months vs. 8 of 23 eyes (34.8%) that were medically managed.
■ Noninfectious corneal ulceration and stromal thinning. Investigators used multiple layers of amniotic membrane in 22 consecutive patients (22 eyes) refractory to medical treatment, with a successful result in 20 eyes (91%).10 Mean preoperative residual stromal thickness at the ulcer bed was 222 μm, while mean total corneal thickness (including the amniotic membrane layers) was 623 μm at day one postoperatively. The findings illustrated that multiple layers of amniotic membrane can integrate into the corneal stroma, leading to increased corneal thickness.
I usually have the patient present for follow-up within three days after membrane placement. I confirm the ring is well centered, the patient is comfortable and no exposure keratopathy is present. I typically leave the biological bandage in for 7-14 days. If it has not melted by this time, I will remove it.
When to Use a Graft
While I typically use amniotic membrane for corneal pathology, I will opt for the AmnioGraft amniotic membrane allograft for other anterior segment disorders. The amniotic membrane graft offers the same regenerative effects as ProKera, but it can cover a larger surface. For example, a graft is indicated to prevent recurrence of pterygium as well as to decrease or prevent scarring of the corneal tissue, and help promote healing of the ocular surface. The graft is also indicated for conjunctivochalasis refractory to treatment with topical medications.
I typically use the inlay technique, debriding the wound and then suturing or gluing the amniotic membrane with the epithelium/basement membrane side facing outward. This allows epithelial cells on the cornea to migrate onto the amniotic membrane and the wound to begin closing.1 Deep defects, such as corneal ulcers, may require multiple layers. The membrane becomes incorporated into the cornea permanently.
In another technique, the onlay technique, the surgeon places a large amniotic membrane on the cornea as a temporary patch that typically detaches from the corneal surface after one to two weeks.1
Whenever I use a graft, I always see the patient at day one postoperatively, at one week and at one or two weeks to monitor healing. During this period, I look for the tissue to melt and become incorporated into the ocular surface.
AMT in Treating Infectious Keratitis
A number of trials and reports have documented the efficacy of amniotic membrane in treating varied forms of infectious keratitis. One study compared 14 eyes with Pseudomonas that underwent AMT group to 11 eyes in controls found the former exhibited less pain and earlier healing of corneal epithelial defects, while the sizes of corneal opacities and neovascularization were similar.11 The AMT group reported better uncorrected visual acuity.
In another study, investigators in France found that early AMT combined with topical corticosteroids in severe BK provided immediate pain relief and allows epithelial healing.12
In a prospective noncomparative case series, 12 patients with severe bacterial keratitis received maximal topical antibiotics, then underwent amniotic membrane transplant at 48 hours. They reported a significant decrease in pain score, and achieved epithelial healing within eight to 45 days.
Use AM Early
Perhaps the most significant take-home message I can offer based on these studies and my own clinical experience is that early use of amniotic tissues is key in treating severe ocular inflammation rather than waiting until the patient has a chronic anterior segment problem that has lingered without improvement. Earlier use means less likelihood of scarring and less likelihood of irreversible chronic changes in the eye. OM
References
1. Meller D, Pauklin M, Thomasen H, Westekemper H, Steuhl KP. Amniotic membrane transplantation in the human eye. Dtsch Arztebl Int. 2011;108:243-248.
2. Liu J, Sheha H, Fu Y, et al. Update on amniotic membrane transplantation. Expert Rev Ophthalmol. 2010 5:645-661.
3. Thatte S. Amniotic membrane transplantation: an option for ocular surface disorders. Oman J Ophthalmol. 2011;5:67-72.
4. Trattler WB. Promoting corneal wound healing. Cat Refrac Surg Today. 2012;July:(insert)1-4.
5. Sheha H, Liang L, Li J, Tseng SC. Sutureless amniotic membrane transplantation for severe bacterial keratitis. Cornea. 2009;28:1118-1123.
6. Yildiz EH, Nurozler AB, Ozkan Aksoy N, Altiparmak UE, Onat M, Karaguzel H. Amniotic membrane transplantation: indications and results. Eur J Ophthalmol. 2008;18:685-690.
7. Celik T, Katircioglu YA, Singar E, et al. Clinical outcomes of amniotic membrane transplantation in patients with corneal and conjunctival disorders. Semin Ophthalmol. 2013;28:41-45.
8. Iakimenko SA, Buznyk OI, Rymgayllo-Jankowska B. Amniotic membrane transplantation in treatment of persistent corneal ulceration after severe chemical and thermal eye injuries. Eur J Ophthalmol. 2013 [Epub ahead of print].
9. Hsu M, Jayaram A, Verner R, Lin A, Bouchard C. Indications and outcomes of amniotic membrane transplantation in the management of acute Stevens-Johnson syndrome and toxic epidermal necrolysis: a case-control study. Cornea. 2012;31:1394-1402.
10. Nubile M, Dua HS, Lanzini M et al. In vivo analysis of stromal integration of multilayer amniotic membrane transplantation in corneal ulcers. Am J Ophthalmol. 2011;151:809-822.
11. Barequet IS, Habot-Wilner Z, Keller N, et al. Effect of amniotic membrane transplantation on the healing of bacterial keratitis. Invest Ophthalmol Vis Sci. 2008 Jan;49:163-167.
12. Gicquel JJ, Bejjani RA, Ellies P, Mercié M, Dighiero P. Amniotic membrane transplantation in severe bacterial keratitis. Cornea. 2007;26:27-33.
